Southern California dealing with a trio of viruses this winter — and yes, one of them is COVID – Daily News
Now would be a good time to stock up on cough medicine, tissues and tea – as a trio of viruses is making the winter season miserable for Southern California residents and health care professionals.
Coronavirus transmission, just like every winter since 2020, has once again increased as temperatures have declined, though not quite to the level of last year’s surge. Then there’s influenza and respiratory syncytial virus – or RSV – which, health care professionals said this week, have returned with a vengeance.
The causes of the triple spike, according to health officials, are fairly prosaic: Viruses generally thrive in cold weather. Holiday gatherings are a human buffet for viruses. And, after three years of intense diligence about being inoculated against the coronavirus, vaccine fatigue has set in.
The result is that the number of people contracting one or more of these respiratory viruses has been on the rise since before Christmas. And even though the severity is nothing like the carnage seen at the height of the coronavirus pandemic, emergency room visits are up – and hospitals are feeling the pressure.
“We started to see more respiratory illnesses the week before Christmas,” Dr. Suman Radhakrishna, an infectious disease specialist with Dignity Health California Hospital, said in a Thursday, Jan. 4, interview. “It was a mishmash of a lot of different things.”
Public health agencies use a smattering of metrics, aside from just a total count of new COVID-19 cases, to determine the full breadth of coronavirus spread in a given region. And for many Southern California health care providers, most of the metrics have been on the upswing over the past few weeks.
In Los Angeles County, for example, there were 542 new COVID-19 cases reported daily, on average, this week, a decrease from the 621 daily average cases reported last week.
But, according to the LA County Department of Public Health, the decrease is likely because a fewer number of reportable tests were conducted during the holidays. A majority of folks also self-test at home and don’t report positive results to the county, DPH said.
Wastewater concentration, though, has increased notably since last week, DPH said.
That metric, which is the amount of COVID-19 detected in sewage water, provides public health agencies with a better understanding of how COVID-19 is spreading – and its potential to strain the health care system.
LA County’s wastewater concentration this week was 49% of last year’s winter COVID-19 surge, a substantial peak from the 36-39% reported over the past three weeks.
The metrics in Pasadena and Long Beach, both of which have their own health departments, are similar, as are those in Orange County, though on a smaller scale.
The good news, though, is that the metrics are nowhere near the levels reported during the height of the pandemic, Radhakrishna said – and the symptoms, generally, are not as severe.
“We’re not seeing that, and I hope we never do again,” Radhakrishna said about coronavirus transmission this winter compared to past years. “Now, (COVID-19) is behaving like a bad head cold.”
But the rising coronavirus metrics do not exist in a vacuum. Instead, increased coronavirus spread has coincided with a rise in influenza and RSV transmission.
Some patients, in fact, have been diagnosed with multiple viruses at once.
When combined, the respiratory viruses can also cause more severe problems, Radhakrishna said, particularly for those with underlying health problems, such as heart disease or diabetes.
“They are sick like dogs because they have two infections rather than one,” she said. “People will recover from it — but it takes a longer period of time.”
Flu and RSV, like the coronavirus, have also been detected at greater levels in LA County, with 22.9% of tested samples positive for the flu and 10.3% positive for RSV, according to DPH data for the week ending on Dec. 23.
It’s much the same in Long Beach and Pasadena.
The situation in Orange County, meanwhile, is not as severe. The Orange County Health Care Agency’s latest data indicates 8.3% of influenza lab tests were positive, after peaking the week prior at 8.9%. The RSV positivity rate crescendoed at 9.5% in the last week of November and was at 7.9% this week.
The coronavirus, influenza and RSV triad, meanwhile, have caused hospital visits and admissions to increase as well.
At Pasadena’s Huntington Hospital, for example, coronavirus infections have steadily climbed since mid-November, and the facility had 38 COVID-19-positive patients this week — six of whom were in the intensive-care unit.
But this year, officials said, the flu and RSV are causing the more severe symptoms.
“Influenza as well as RSV have definitely come back with a vengeance,” Dr. Thomas Yadegar, the medical director of Providence Cedars-Sinai Tarzana’s intensive care unit, said on Thursday, noting that many hospitals are hitting capacity as folks with those viruses flood emergency rooms.
About 10.5% of all emergency department encounters in the county were for influenza-like illnesses for the week ending Dec. 23, DPH said.
But while influenza and RSV are increasingly problematic, COVID-19 is still dominant among the triumvirate.
LA County, for example, had an average of 783 people admitted to hospitals with a positive COVID-19 diagnosis this week, up from 690 per day the week prior.
Hospitalizations related to COVID-19, in fact, have increased significantly since late December, to the point that the county on Dec. 27 moved into the “medium” admissions category, as determined by the U.S. Centers for Disease Control and Prevention.
The CDC has a three-tiered system to help public health agencies determine COVID-19 transmission levels and their impact on the health care system.
It also has set public health protocols in relation to each tier, which are low, medium and high.
LA County hit the medium tier in late December after its COVID-19-related hospital admissions topped 10 per 100,000 people daily.
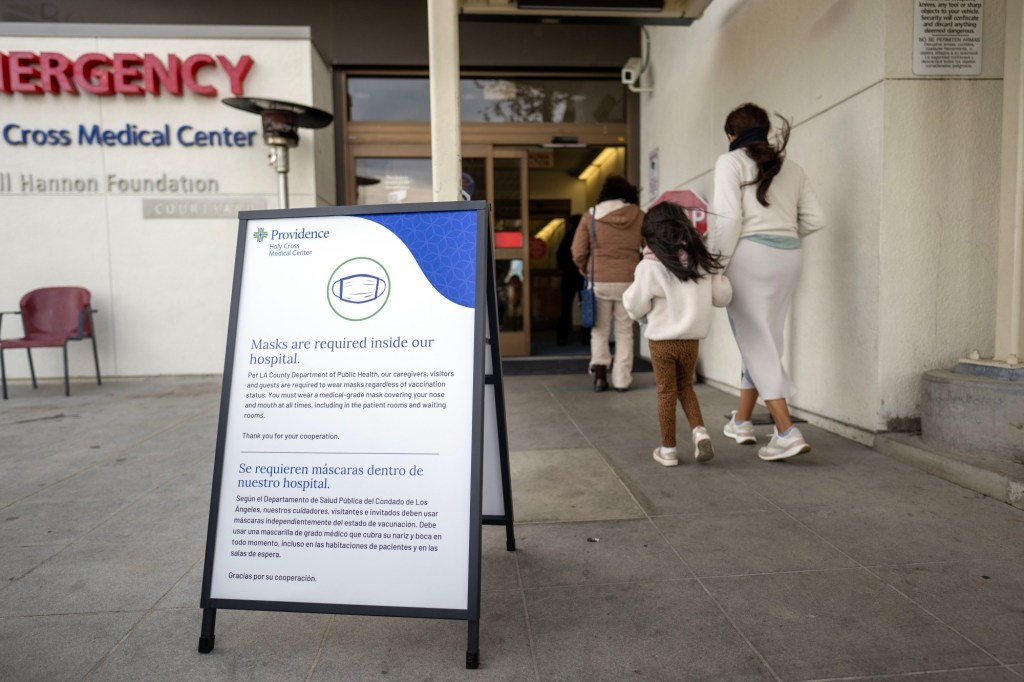
As a result, all health care personnel working in licensed facilities providing inpatient care are now required to wear a mask when in contact with patients or in patient-care areas, according to DPH.
The masking requirement will be lifted when the county’s numbers drop below the medium hospital admissions level.
Orange County’s hospitalization levels also recently passed into the medium tier, according to Dec. 30 data, which showed that 320 people were admitted to the hospital for COVID-19 during the most recent reporting period — a 19% jump from the week prior.
Southern California isn’t alone.
Hospitals across the country are also feeling the brunt of the viral triumvirate, with high levels of flu-like illness reported in 31 states just before Christmas. Many health care facilities have now begun requiring patients, visitors and personnel to once again wear masks to help prevent additional cases of each virus.
“What you’re hearing is unfortunately true,” Yadegar said. “There’s definitely been an increase in influenza cases, as well as COVID.”
The respiratory illnesses, though, aren’t just taking their toll on patients, Yadegar said – but also hospital staffers and doctors.
“So many nurses have fallen sick,” he said. “We’ve had a lot of nurses not able to come to work. Many are working extra shifts — and that makes it tougher.”
Vaccine fatigue is also an issue.
Vaccinations for all three diseases are down this year, according to CDC data. That could be a contributing factor to the viruses’ increased visibility this season, health care professionals said, even though natural immunity has helped keep transmission from spiking out of control.
About 44% of U.S. adults had gotten flu shots by Dec. 23, according to the most recently available CDC data. Only about 19% of U.S. adults were reported to have received an updated COVID-19 shot as of early December.
“That’s probably one of the reasons we’re seeing quite a bit of disease,” said Dr. Kimberly Shriner, Huntington Hospital’s infectious disease and tropical medical specialist. “I think people have kind of gotten that vaccine fatigue.”
Some folks, Shriner added, may be under the false impression that the first rounds of the COVID-19 vaccine were enough to protect them from the disease for a lifetime.
“Unfortunately, it’s just gonna be like the flu — in fact, even maybe a little bit more challenging than the flu,” Shriner said, “since you have to get vaccinated every six months to certainly every year.”
Radhakrishna agreed about the fatigue.
“I get it,” she said. “I’ve been jabbed so many times I’m tired of it, too — but people kind of forgot about influenza and COVID.”
Public agencies, from Los Angeles to Orange counties, have fought against complacency, repeatedly encouraging folks to stay updated on all vaccines, and to get tested for COVID-19 frequently.
“With higher COVID-19 transmission levels in Los Angeles County – along with other respiratory viruses – and many residents returning to school and work after the holidays,” DPH said in a Thursday news release, “(DPH) is encouraging residents to test if they have COVID-19 symptoms to prevent the spread of COVID-19.”
Those who get a positive COVID-19 result — especially folks with underlying health conditions — should consider their medication options as soon as possible.
Antivirals, including Paxlovid, can help treat symptoms more quickly and reduce the risk of long COVID, according to DPH.
But that drug isn’t for everyone, according to Radhakrishna — and many patients have reported not liking the drug because of its strong taste.
“Is (Paxlovid) being used as much as we’d like it to be used in the community? Probably not,” Radhakrishna said. “But it is being used.”
Health officials are also urging folks to consider masking indoors — especially in crowded spaces — to avoid catching any of the winter respiratory illnesses currently circulating.
And if you’re feeling sick, stay home.
“As we enjoy the winter season and enjoy more indoor activities,” Jennifer Bayer, a spokesperson for Tenet Healthcare, which includes hospitals in Fountain Valley, Los Alamitos and Placentia, said in a statement, “we urge our community to proactively protect themselves and others by staying home when they feel under the weather, wearing a mask when possible and using good hand hygiene.
Having a handy supply of cold medicine and tissues wouldn’t hurt either.
For more information about COVID-19 vaccines and testing, visit myturn.ca.gov and ph.lacounty.gov/COVIDtests.
Staff writers Ryan Carter and Michael Slaten, as well as the Associated Press, contributed to this report.